This is a big piece of what the “vaccines-cause-autism” idea is built on. Really bad analyses. Another study shows up showing that vaccines don’t cause autism. People immediately jump to give talking points to their community: “ignore this study! In fact, it’s just another conspiracy to defraud you!!!!!”*
But they know from history, their community doesn’t check. They don’t test whether the talking points hold up. Either that, or they really are this bad at simple math.
One reason I slowed down a lot on writing debunks of the “vaccines cause autism” community is that it’s very repetitive. It only takes a few minutes to see where they make their mistakes. I admit, I have the training and the time to do that checking, but it leaves me wondering. As in, it’s hard to not ask: “are they really this bad at science? Are they so biased they don’t know they are wrong? Or, are they lying?” I don’t know. What matters most is they are wrong. I am grateful that I had the time to spend checking their claims and was able to not get sucked into that world.
That intro aside, there was a recent study that, once again, shows that the MMR vaccine doesn’t increase autism risk. 21 years since Wakefield’s junk study and we are still spending time and money countering his misinformation. When you look at what the autism community needs, it’s just sad to see resources used this way. But I get it. The anti-vaccine community is doing real harm (note the rise in measles in the US and elsewhere). But, dang, I’d like more work done to help my kid.
So, what’s this new study? Measles, Mumps, Rubella Vaccination and Autism: A Nationwide Cohort Study. With the conclusion:
The study strongly supports that MMR vaccination does not increase the risk for autism, does not trigger autism in susceptible children, and is not associated with clustering of autism cases after vaccination. It adds to previous studies through significant additional statistical power and by addressing hypotheses of susceptible subgroups and clustering of cases.
Thanks for doing this, but, again, the results are not surprising in the least.
Naturally this brought about a big response from the anti-vaccine community. The go-to place for defense of “vaccines cause autism” used to be the Age of Autism blog. I went there and found they just recycled a piece from a guy named James Lyons Wieler. Apparently he was once a scientist, but he now seems to be a guy asking autism parents for money to write bad articles about how vaccines cause autism. In this case has found the “Smoking Gun” for why the MMR study is so wrong.
(1) The smoking gun is the study-wide autism rate of 0.9-1%. The rate of ASD in Denmark is 1.65%. Where are the missing cases of ASD? Given past allegations of this group’s malfeasance and fraud, the rest of the study cannot be accepted based on this disparity alone: the study group is not representative of the population being studied.
Clearly they must be fudging the data!!!!!
This appears to have become the talking point that the anti-vaccine community is passing around. It was picked up by Brian Hooker. He wrote “A Scientist’s Rebuttal to the Danish Cohort Study“:
1. Children were notably missing from the study sample:
First and foremost is the underascertainment of autism cases within their data sample. The study authors used Denmark population registries of children born in Denmark of Danish-born mothers which should reflect the current reported autism incidence in Denmark at 1.65% (Schendel et al. 2018, JAMA). However, the autism incidence within the sample of the Hviid et al. paper is 0.98%, meaning that approximately 4,400 autistic children are missing from this study. The authors do not discuss the discrepancy in the number of cases.
Again, his number 1 point, the missing children!
Even JB Handley (remember him? Yes, he’s back) wrote about this. Focusing his whole piece on this “missing” group in the MMR study: New Danish MMR study shows autism rate of 1 in 100—CDC should rush to Denmark!
2. The most compelling data in the study will never get covered: why is the autism rate in this study only 1 in 100?
Here in the U.S. we’re at 1 in 36! Shouldn’t CDC researchers rush to Denmark to figure out why their autism rate is so much lower than ours? For every 1,000 Danish kids, only 10 have autism. But here in the U.S., we have 28 per 1,000, that’s 177% more autism! I thought Paul Offit wanted everyone to believe the autism rate was the same everywhere? What gives?
Hold on to your seat, Handley. It’s about to get discussed.
I had thought I’d take the easy route and just email the study author for an explanation. That could have answered the big question for Handley, Weiler, and Hooker. But that would take a day or two to get a response from Denmark. Why not just, you know, read the paper? Or, just the introduction?
Under the “Abstract” section of the MMR paper, which has the “missing” autistic kids and a lower prevalence rate:
Participants: 657 461 children born in Denmark from 1999 through 31 December 2010, with follow-up from 1 year of age and through 31 August 2013.
Under the methods section for the earlier Denmark paper, which has the higher prevalence rate:
All live births in Denmark between 1980 and 2012 were identified in the Central Person Register and followed through 2016 for an ASD diagnosis
It’s not that hard to compare the two studies.
One study looked at Danes born from 1999 to 2010. And took data from 2013. This is the MMR study.
The other study looked at Danes born from 1980 and 2012. And took data in 2016.
Apples, meet Oranges.
Seriously, people are surprised that they came to different answers as to the overall prevalence? I mean, this is your “smoking gun”? This is the best the “vaccines cause autism” community can do? If nothing else, one study took data later than the other. You are the “it’s an epidemic!” team, surely you accept that the autism rate is higher in the later dataset.
But, hey, this didn’t take the full 5 minutes I allocated to check the claims of this “smoking gun” against this new study. I still had 4.5 minutes.
So, let’s see if the data really are compatible. Can we take the data from the prevalence study and get the same number as in the MMR study? Yes, I’m a geek and this is what I do. But we just saw that 2 Ph.D.’s (Hooker and Wieler) and a business guy (Handley) didn’t think to do that. Is it really that hard? (I do wonder how Handley made money. Seems like he must have relied on someone else to do the numbers.)
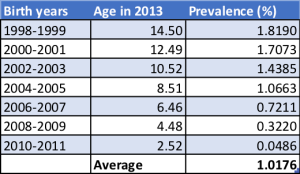
I just wrote about the autism prevalence study: Yes, there are a lot more adult autistics than commonly thought. The real question is what we do with this information. I have the graph from the prevalence study, so I ran the numbers quickly. If we limit ourselves to the autistics in the MMR study (born 1999 to 2010) and take data in 2013, we get a prevalence value of 1.02%.
1.02% using the prevalence study. Compared to 1% in the MMR study.
They are the same. No “malfeasance”. No “fraud”. No “discrepancy”. And, Mr. Handley, no evidence you can use to blame the HepB vaccine for autism.
Now for the dull part. Here’s my math.
Step 1: I digitized the graph. The red points are where I took prevalence data from the graphs. Each line represents 2 birth years, so I took points where for the age of the average kid in each cohort in 2013.
Here’s the summary table from those data points.
I did this fast. Let me know if I made a mistake. That’s why I’m showing my work. It’s not precise because, well, it’s done by hand. Also, there’s the fact that the MMR paper was for kids born from 1999 to 2010. The prevalence study has kids grouped by 2 years. So I have data for 1998-99 where I only really want 1999. It’s good enough. The “age in 2013” is what the digitizer gave me for the datapoint positions I chose. I can’t get exactly, say, 10.5. But, again, it’s good enough.
Anyway, there’s no “smoking gun” as James Lyons Weiler says. There aren’t children “notably missing” as Brian Hooker claims. And the “most compelling data” according to JB Handley is just that he can’t read a scientific paper.
This is a big piece of what the “vaccines-cause-autism” idea is built on. Really bad analyses. Another study shows up showing that vaccines don’t cause autism. People immediately jump to give talking points to their community: “ignore this study! In fact, it’s just another conspiracy to defraud you!!!!!”*
But they know from history, their community doesn’t check. They don’t test whether the talking points hold up. Either that, or they (people like Handley, Hooker and the rest) really are this bad at simple math.
—
By Matt Carey.
*Yeah, you guys are pushing a conspiracy theory. I know you like to say “oh, he called us conspiracy theorists, therefore we don’t have to listen to him.” Surprise me. Grow a backbone and defend the points in this commentary rather than either (a) ignoring it or (b) dismissing it because I pointed out that you are claiming scientists conspired to fool the world.













Recent Comments